12th April 2020 – Immunity is the key to live or die in COVID-19
A Blog by Dr David J Flavell PhD FRCPath
Charity & Scientific Director of Leukaemia Busters
12th April 2020
COVID-19 Immunity: Kill or Cure?
Immunity is the key to live or die in COVID-19
-
The immune system that protects us is complex and efficient but does make mistakes.
-
The lung damage in COVID-19 is due to a damaging inappropriate immune response.
-
Understanding the damaging immune mechanisms behind COVID-19 will be a game-changer
The immune response we mount against the SARS-CoV-2 virus, the cause of the COVID-19 illness, is a double edged sword. In the majority of people, immunity develops and they get better. However, an unfortunate 20% develop severe symptoms with breathing difficulties that can, in around a quarter of these, lead to a fatal viral pneumonia and death even when the most advanced medical life support is given.
So what is it about this viral disease that makes it so severe in some but not in others, a disease where some individuals suffer only the mildest of symptoms whilst others end up on ventilators fighting for their lives?
The severe reaction to the COVID-19 virus usually doesn’t happen during the first week of infection but more often during the second week or even later, hence the time lag we see between initial infection and death some weeks later.
So what might be going on?
Why is it that some sail through the infection with just bad cold-like symptoms whilst others end up fighting for their lives in intensive care units on ventilators?
All evidence points to our own immune system being the culprit and I’ll explain what that might actually mean and how understanding the precise mechanism behind this will likely change everything and allow us to develop targeted drug treatments that will counter the severe life-threatening symptoms.
Attack and Protect
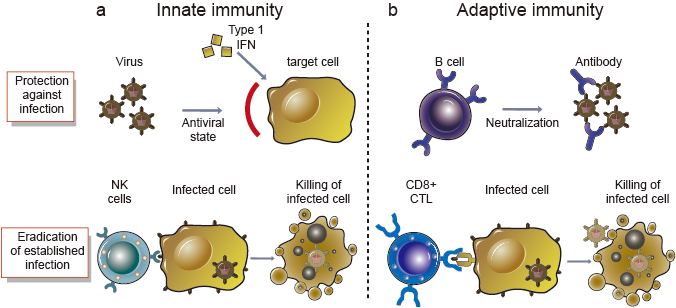
When we become infected by any microorganism, be it a bacteria, virus or fungus, the first thing that immediately kicks in is our innate immune system as the first line of defence. Certain types of innate white blood cells, one of the most important being natural killer cells (NK cells) recognise some of the molecular patterns displayed by the invading microorganism and go on the attack against them and the cells which they infect.
This system is effective at reducing the burden of infection but often invading microorganisms are able to sneak past, the infection is slowed but still continues on. We then have to rely on another compartment of our immune system called the adaptive immune response that takes 2 to 4 weeks to kick in, as white blood cells called lymphocytes (B cell) undergo some amazing internal genetic changes in preparation to produce antibodies that act as little guided missiles aimed very precisely at the invading microorganism.
Alongside antibody producing lymphocytes another type of lymphocyte called a cytotoxic T-cell (CTL) also undergo internal genetic changes that allows these cells to recognise and home in on the invading microorganism or cells infected by it and then destroy these cells.
Put in a very simple way that’s how our highly complex immune system works, it is a very potent killing machine that works extremely efficiently the vast majority of the time protecting us from from the myriad of microorganisms surrounding us in our daily lives.
Without it we would be overwhelmed by microorganisms very quickly. Because our immune system is so potent, if it does goes awry for whatever reason, going on the attack against our own tissues and organs then it can cause enormous problems in the form of autoimmune diseases such as rheumatoid arthritis, ulcerative colitis or multiple sclerosis.
Immune Mayhem
Immunologists, scientists like myself who study immunity and the immune system (in my case usually in the context of blood cancers) are just beginning to understand how the SARS-CoV-2 virus that causes COVID-19, likely causes the damage it does to the unfortunate 20% or so of individuals who develop severe, sometimes life-threatening symptoms.
There are several theories for this, some for which there is good scientific evidence, evidence that continues to build as immunologists study the disease in greater detail as this pandemic progresses across the world. From these studies there is a general consensus forming that the serious damage to lungs and other organs in patients with severe COVID-19 is driven by an inappropriate immune response to the virus and there are clues building as to how this actually occurs.
One of the common things that happens in the majority of COVID-19 patients is that the white cell called lymphocytes circulating in their blood decline in number as the infection progresses. It is thought that this happens because their lymphocytes migrate out of the blood and into the lungs in response to the myriad of viral particles there are present in the cells of the respiratory tract.
As the lymphocytes sit there in the lungs adapting themselves to launch an attack on the virus (remember this can take between 2 – 4 weeks), the virus actually turns the tables and invades the lymphocytes in which they then begin to replicate so rapidly that they burst the lymphocytes wide open resulting in a massive spillage from the lymphocytes interior of special immune messenger chemicals called cytokines. This whole abnormal and damaging pathological process is technically termed pyroptosis.
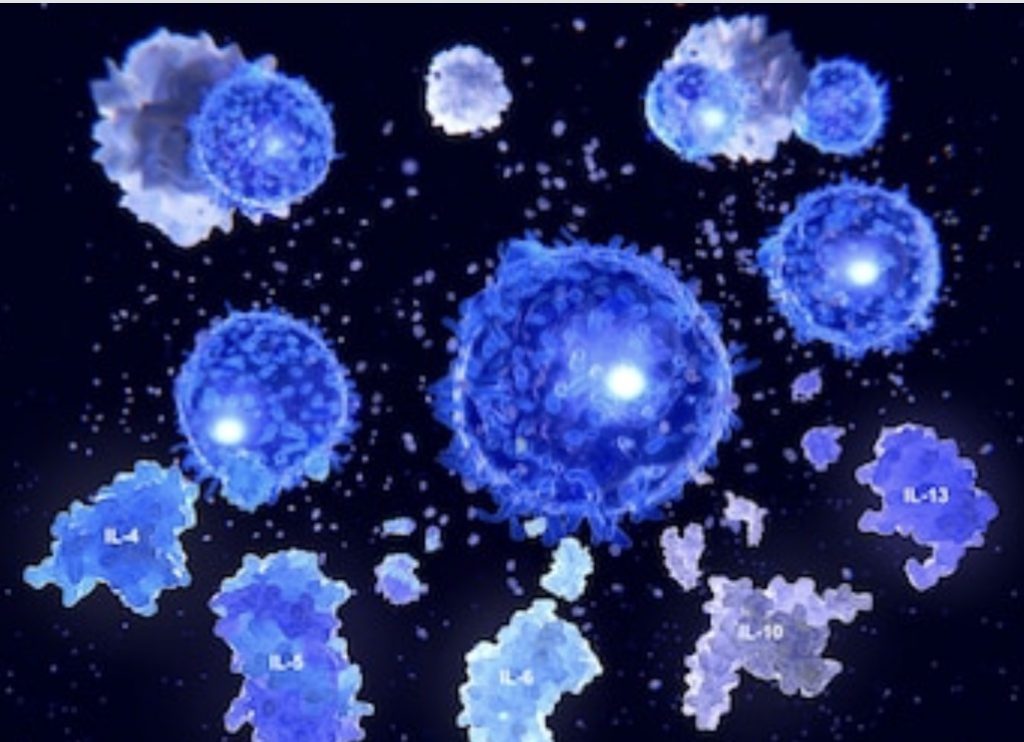
Cytokines are the chemical messengers of the immune system that normally orchestrate a finally tuned immune response and it is the mass uncontrolled spillage of these from virus infected lymphocytes that is thought to be, at least in part, behind the extensive and deadly inflammation that occurs in the lungs and elsewhere in some patients with COVID-19 infection.
An Urgent Question
The urgent question that will eventually be answered by immunologists and other biomedical scientists is,
why do some individuals and not others progress to develop fatal lung damage due to pyroptosis or some other immunological mechanism?
There are a whole range of possibilities here. It may be that there is a genetic predisposition for some individuals, due to as yet unidentified inherited genes or it may be that in some individuals their immune systems may have been primed in such a way by prior exposure to various types of microorganisms in the past (including other coronaviruses that cause nothing more than a common cold) to respond in an inappropriate and fatally damaging way.
The latter may explain why the older you get the more likely you are to develop severe and fatal symptoms simply because older people have encountered many more microorganisms during their lifetimes than younger people, in which case the older persons immune systems may be more likely primed in a state to respond in a more damaging way.
These are just some of the possibilities, there are others that are currently or have yet to be investigated in laboratories around the world, all with the same common goal, to defeat the COVID-19 virus.
The global scientific chase is now on to find the answers and be assured that when they do arrive and we understand the mechanism(s) behind this health conundrum that will also likely give us valuable biomarkers, identify new drug targets and change everything for the better.
To read our other blogs click here.
For an up to date on our COVID-19 blog please follow us on Twitter:


