2nd June 2020 – What Can COVID-19 Teach Us About the Cause of Childhood Leukaemia?
A Blog by Dr David J Flavell PhD FRCPath & Dr Sopsamorn (Bee) Flavell BSc PhD
Scientific Directors of Leukaemia Busters
2nd June 2020
Childhood Leukaemia and COVID-19
The COVID-19 pandemic may well lead to both a global increase and decrease in cases of childhood leukaemia that could teach us something important about the actual cause.
For over 100 years there has been the suspicion that a common, though yet to be identified, infection is responsible for the cause of leukaemia in children. This suspicion has arisen because an acute “viral type” infection in a child often precedes the emergence of leukaemia weeks or months later.
9 year old Simon Flavell in 1989 (1980-1990)
Ask almost any parent who has had a child with leukaemia and they will tell you anecdotally that their child was ill with a high fever, sometimes with enlarged lymph glands before they developed the leukaemia. We were no exception, our little boy Simon was very poorly to the extent that he was bed bound with a high temperature, night terrors and most disturbing of all enlarged lymph glands throughout his body indicative of a generalised immune reaction. This went on for over three weeks. He seemed to recover well from that infection but then over the next month or two he developed a slowly emerging form of childhood leukaemia.
It is easy to believe, particularly if you are the parent, that such an acute infection shortly before the appearance of leukaemia in your child was the cause but as with most things in the biological world this is probably too simple an explanation. A lifetimes work carried out by Professor Sir Mel Greaves at London’s Institute of Cancer Research offers an alternative explanation and it is one for which the evidence is growing year by year. Strangely enough the COVID-19 pandemic may provide vital clues and information that will contribute to understanding this process and help provide answers to this most perplexing of questions.
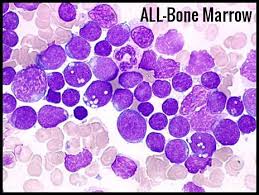
Acute Lymphoblastic Leukaemia (ALL) in the bone marrow
Science progresses through a process termed hypothesis testing which simply put means that a scientist proposes a reasoned explanation to explain a particular phenomenon, based on observation. It is then the scientist’s job to conduct experiments to test that hypothesis to see if it is correct or not. This is at the heart of all scientific investigation and is the reason that you and us have mobile telephones, the internet, aircraft and effective medicines.
The “two hit” Hypothesis
The hypothesis proposed by Greaves for the most common form of childhood leukaemia (termed pre-B cell acute lymphoblastic leukaemia, referred to hereafter as ALL) is that leukaemia arises as a result of two different events or the “two hit” hypothesis.
-
The first hit occurs following damage to a key gene or genes in a single white blood cell when the child is still in the womb.
Such damage may be due to a natural spontaneous error occurring when a precursor blood cell in the developing foetus divides or to the mother’s exposure to an environmental genotoxin (something such as a chemical or X-rays that cause genetic mutations). At least some of these genes and the nature of the damage to them have already been identified in many cases of leukaemia with the most common having the catchy name ETV6-RUNX1, an abnormal joining together of two different genes. This single genetically damaging event in one single cell results in the generation of an identical group, or clone of “pre-leukaemic” cells, which on their own do not develop into leukaemia.
-
The hypothesis states that transformation to a fully malignant leukaemia cell only occurs if there is a “second hit” to that silent pre-leukaemic clone at some point in time after the child has been born.
Greaves hypothesis is that one or more common infections can provide the second hit that tips the balance, transforming the pre-leukaemia cells from a quiescent to a fully malignant state and the resultant clinical emergence of leukaemia in the child.
Microbiome Concept
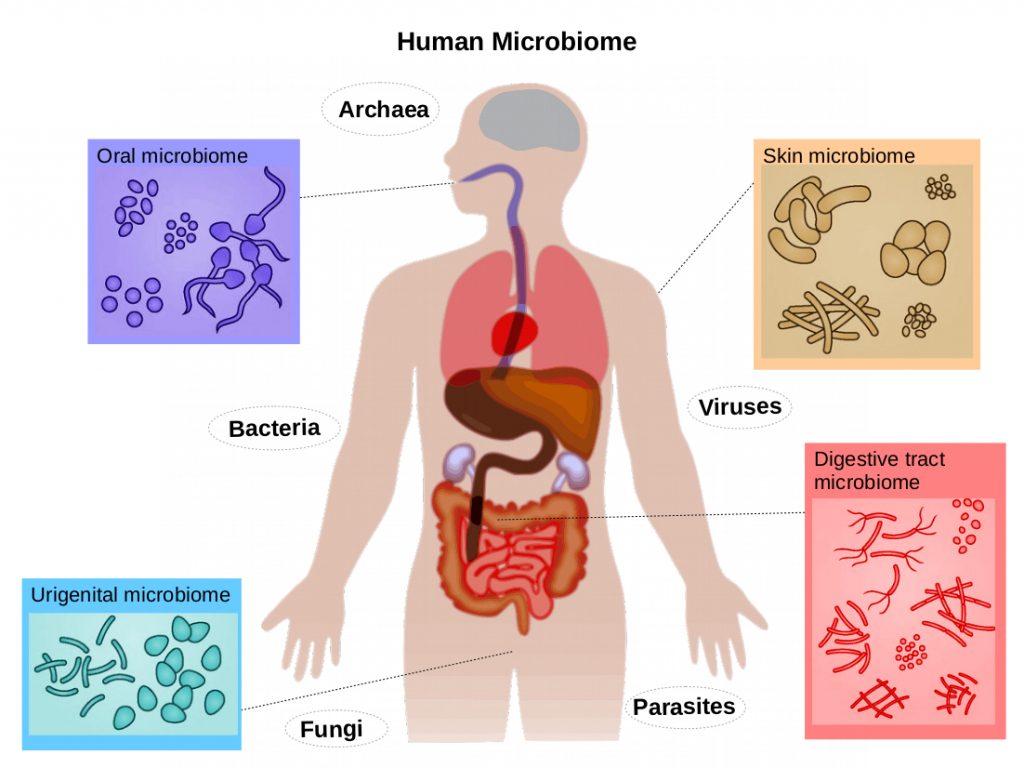
An additional crucial and paradoxical aspect of the infection hypothesis is that children who have a diminished exposure to microbes during early life are more prone to developing leukaemia. It is now understood that the immune systems of new-borns actually requires exposure to benign and beneficial microbes (technically termed the microbiome) in order to perform optimally.
This then ensures that subsequent exposures to infections prompt a well-regulated normal immune response rather than chronic inflammation or an abnormal immune response that itself becomes the second hit trigger for ALL.
In favour of this concept are epidemiological observations which reveal that the risk factors for childhood ALL are surrogates for how infants acquire their essential microbiomes right at the beginning of their lives. These include mode of birth (caesarean section or natural birth), breast feeding and social contacts in infancy.
How might the COVID-19 pandemic affect the incidence rates of childhood leukaemia on the global stage?
That’s the Greaves hypothesis in a nutshell for which there is a growing list of scientific evidence to back it up. This being the case how might the COVID-19 pandemic affect the incidence rates of childhood leukaemia on the global stage? This hypothesis allows for two sharply contrasting possibilities.
- The first is that COVID-19 infection in children, though generally very mild or even asymptomatic, might be expected to provide the second hit that leads to a higher incidence of leukaemia in those children already carrying the genetic damage that they acquired from the first hit in the womb. It is highly relevant here to realise that spikes in ALL incidence occur a few months after epidemics of seasonal flu.
- But then sharply contrasting with this is the idea that nursery and school closures during the pandemic have changed the dynamic. A significant number of very young children have been isolating at home and have thus avoided the second hit they might otherwise have received had they been mixing freely with their peers. In this instance the hypothesis would predict a reduced incidence rate of childhood leukaemia and indeed this is exactly what happened in Hong Kong when schools were closed for a year during the 2003 SARS outbreak there.
So paradoxically the COVID-19 pandemic might be seen to cause both an increase and decrease in the incidence of childhood leukaemia depending on the prevalent circumstances in different countries and societies. The information that emerges on this issue over the coming months and years following the COVID-19 pandemic will inch us further forward in understanding and working out the cause of childhood leukaemia, a step that may well allow the development of interventions to actually prevent this.
All hope is pinned on the possibility that the most common form of childhood leukaemia may be preventable once we fully understand the mechanism that is the cause of this malignancy. As terrible as the COVID-19 pandemic has been it will have taught us valuable lessons and provided positive benefits to the future of new medical breakthroughs of which the childhood leukaemia story is but one.

Some young leukaemia patients at Southampton General Hospital
Thank you for following our blogs and for your support during these extremely difficult times for all of us.
To read our other blogs click here.
For an up to date on our COVID-19 blog please follow us on Twitter:



